Pulmonary Embolus Lawsuits
Death by Preventable Post-Operative Pulmonary Embolus
A 65-year-old woman undergoes a very routine outpatient knee arthroscopic surgery. The surgery goes well and the patient is discharged with expectation of a short and uneventful recovery at home. But two days later, she collapses and dies. An autopsy confirms the patient died of a blood clot that lodged in the artery leading to the lungs, known as a pulmonary embolus [PE].
In 2022, the United States Center for Disease Control and Prevention [CDC], reported that as many as 900,000 Americans suffer a PE every year, resulting in 100,000 preventable deaths. In the same report the CDC found that 50% of these pulmonary emboli happen either during or shortly after a hospitalization or outpatient surgical procedure. According to the CDC, as many as 70% of these PEs could have been prevented through the use of simple, low-risk prophylactic procedures, particularly the use of anticoagulant drugs. Sadly, though, less than half of hospitalized patients receive anticoagulant drugs. 1 Other very reliable resources report that fatal pulmonary emboli are the number one leading preventable cause of death following hospitalization and surgery, and that up to 99% of fatal pulmonary emboli could be prevented through the appropriate use of anticoagulant medications. 2
Medical literature has been extensive on the importance of assessing and addressing these risks, but far too often health care providers seem not to be getting the message. Lawsuits against health care providers who fail to recognize and address these risks are filed every year across the United States, and these lawsuits continue to be a critical part of the solution in highlighting the need for every health care provider to appreciate and address these horrific risks to their patients.
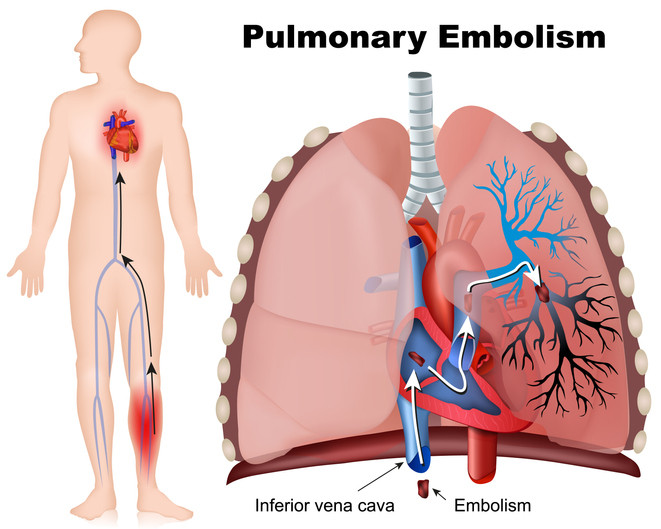
I. What is a pulmonary embolus?
Blood clots that lead to PE are referred to as a “venous thromboembolism,” “VTE,” or a “deep vein thrombosis,” “DVT.” DVTs usually form in the lower legs for reasons explained below. A part of the DVT can break off and travel through the venous system to the heart. The pumping action of the heart causes the clot to travel from the heart to the artery that sends blood to the lungs for oxygenation. As the artery narrows, the clot can no longer pass, and then becomes a PE, which blocks the continued flow of blood through the artery. The inability of the blood to continue its journey to and from the lungs results in the vital organs of the body being deprived of oxygenated blood, causing organ death if not very quickly corrected.
II. What causes DVT and PE?
Blood travels in a continuous loop from the heart, going out through the arterial system and returning through the venous system. Once blood has been delivered to the lower legs through the arterial system, the blood has to reverse direction and travel back to the heart through the venous system. However, this return circulation is made more difficult by gravity. The gravitational force is overcome by the pressure exerted by the pumping of the heart. Circulation back to the heart through the venous system is also greatly enhanced by lower leg movement, such as walking or running, because these activities increase the pressure within the venous system and dilate the veins. Contrarily, blood is not pushed as efficiently back toward the heart when: (a) the patient is immobilized; or (b) return flow is impaired (such as by sitting for long periods of time or later-stage pregnancy). In addition, circulating blood does not tend to clot, but blood stalled in the lower leg veins does tend to clot. Accordingly, when the legs are immobilized and blood is not flowing freely back to the heart, clots tend to form and grow in these lower leg deep veins, DVT. That is the reason it is recommended that folks on long airline trips periodically stand up and walk around.
III. What are the risk factors for the development of a DVT?
As stated above, immobility is a risk factor for development of DVT. There are other risk factors as well. Having a previous history of DVT or PE is widely considered as the most significant risk factor for development of a new DVT. A family history of DVT, PE, or embolic stroke is an independent risk factor. Advanced age (over 60), obesity (BMI over 25), and smoking are risk factors as well. Patients on oral contraceptives also are at higher risk of development of DVT. A significant risk factor is also any prior cancer diagnosis (other than non-melanoma skin cancers). Finally, surgery is a significant risk factor for development of DVT, as explained more fully below.
IV. Why are post-operative patients at risk for development of pulmonary emboli?
During surgery, patients are immobilized. In addition, a number of surgeries require a tourniquet on the leg, which restricts return blood flow. Moreover, after all surgeries patients are immobilized to varying degrees and for varying lengths of time due to pain, discomfort, post-operative weakness, etc. In addition, because the surgeon has cut into some part of the body during the surgery, the body tends to develop clots as a natural mechanism to stop bleeding from the areas of the surgical wounds. But this clotting tendency can and often does cause clots to form not just at the surgical site, but in other portions of the body as well.
V. Can the risk of development of post-operative pulmonary emboli be reliably predicted by assessment of patient-specific risk factors?
Yes, without question. Over the past few decades, researchers have developed forms that can be filled out for patients. Although there are many others, the most widely known and utilized form is the Caprini VTE Risk Assessment form, developed by a pioneer in the field, Dr. Joseph Caprini. This form has been modified and improved numerous times over the years as a result of experience and ongoing research. On all of these forms, each risk factor for the patient is allocated points. At the end of the form, the points are summed, usually from 1-9 or so, and the total points indicate whether the patient needs anticoagulant drugs. It is a very simple process.
The Caprini Scale is readily available for free as an online tool at: https://capriniriskscore.org/assessment/. The paper form for the assessment is freely and widely distributed as well, and a copy of one such form can be found here.
VI. If a patient is deemed at risk of development of a post-operative pulmonary embolism, are there steps the surgical team can take to significantly reduce that risk and how effective are those steps in preventing fatal pulmonary emboli?
Yes, definitely. Patients at the higher risk levels, for example those patients over 60, with a prior history of DVT, a history of cancer, or any other combination of factors that put them at higher risk, should almost always have oral anticoagulant drugs administered for prevention of DVT. As stated above, research has shown that the proper use of oral anticoagulant drugs for high-risk surgical patients can prevent up to 99% of fatalities due to PE.
While anticoagulant drugs do pose a risk of post-operative bleeding, repeated studies have aptly demonstrated the risk of post-operative bleeding for almost all patients on post-operative anticoagulant drugs is actually quite low. For the vast majority of higher patients undergoing any type of surgery, the risk of development of a DVT without anticoagulant drugs is far greater than the risk of bleeding if anticoagulant drugs are appropriately used. Patients with various types of bleeding disorders of course merit further evaluation and weighing of those risks by specialists such as hematologists.
In many minor surgical procedures, such as simple knee arthroscopies, in-patient podiatric surgeries, or even oral surgeries, providers fail to appreciate the risk of DVT and the potentially life-saving efficacy of anticoagulation for higher-risk patients. While the length and scope of the surgery are factors that should be considered, many practitioners fail to take into consideration the other risk factors that may make prophylactic anticoagulation absolutely necessary. This is true even for patients undergoing the most minor surgical procedures. It is critical that a patient who achieves a score mandating anticoagulant prophylaxis receive same. The scoring sheet is simple and readily available and the anticoagulant drugs are inexpensive, low-risk, and widely available. It is irresponsible and an unacceptable patient risk for any health care provider, surgeon, nurse, or facility, to consider the type and length of surgery as the controlling factor in the decision whether an operative patient requires anticoagulant prophylaxis.
VII. Which health care providers face potential legal liability if adequate measures are not taken to reduce the risk of a pulmonary embolus that results in a patient’s death or serious disability?
Ultimately, the surgeon makes the final decision on whether to use anticoagulant drugs on an operative patient. However, the anesthesiologist also may play a role in that decision. In addition, virtually every hospital and surgical center in the United States has adopted a VTE Risk Assessment protocol, in which the nursing staff is required to properly fill out a risk assessment form, like the Caprini form, and to check off the recommended prophylactic regimen depending on the patient’s score. If the scoring indicates the patient should have prophylactic oral anticoagulants but the surgeon does not order same, it is incumbent on the nursing staff to invoke the chain of command so that some physician other than the operating surgeon can participate in the final decision as to whether oral anticoagulants should be used for the high-risk patient. If the hospital or surgical center does not have a proper VTE Risk Assessment protocol, does not use a modern form consistent with current medical knowledge on risk factors and prophylactic measures, or does not adequately train the nursing staff on how to utilize the form properly and invoke the chain of command if it is ignored, the facility and the nurses are potentially liable for any resulting injuries or deaths.
VIII. What should I do in the face of these risks?
If a loved one or you are scheduled for any surgery, go to a website like the one at https://capriniriskscore.org/assessment/, to assess the applicable risk factors. Have a frank discussion with the surgeon as to whether prophylactic anticoagulation is necessary or appropriate for the procedure. Do not allow the health care provider to dissuade you from prophylaxis by contending the surgery is too short or minor to justify the risks. If in doubt, get a second opinion on this specific issue from a qualified specialist, such as a hematologist, cardiologist, critical care physician, or even another surgeon.
If a loved one or you has suffered a serious injury or death from a post-operative PE and was not on anticoagulants, you should obtain the medical records and contact a highly qualified medical malpractice attorney for consultation. Because there are relatively short periods of time in which any suit can be brought, there should be no delay in consulting a qualified lawyer to review your case.